Patient practices are not being fully reimbursed
In an increasingly digital healthcare landscape, the dynamic between patients and clinics is evolving. Amidst this, clinics are pressed to meet patients' expectations for personalized care and more engaged communication, particularly in managing chronic conditions.
With patients increasingly seeking engagement beyond the consultation room, clinics are seeking solutions to keep pace with escalating patient loads, complex communication needs, and their reimbursement rates. Delays in calls and message handling can compromise patient care, especially within Chronic Care Management (CCM), where consistent symptom monitoring and preventative efforts are crucial. An effective chronic care strategy must address both consistent engagement and robust preventative care.
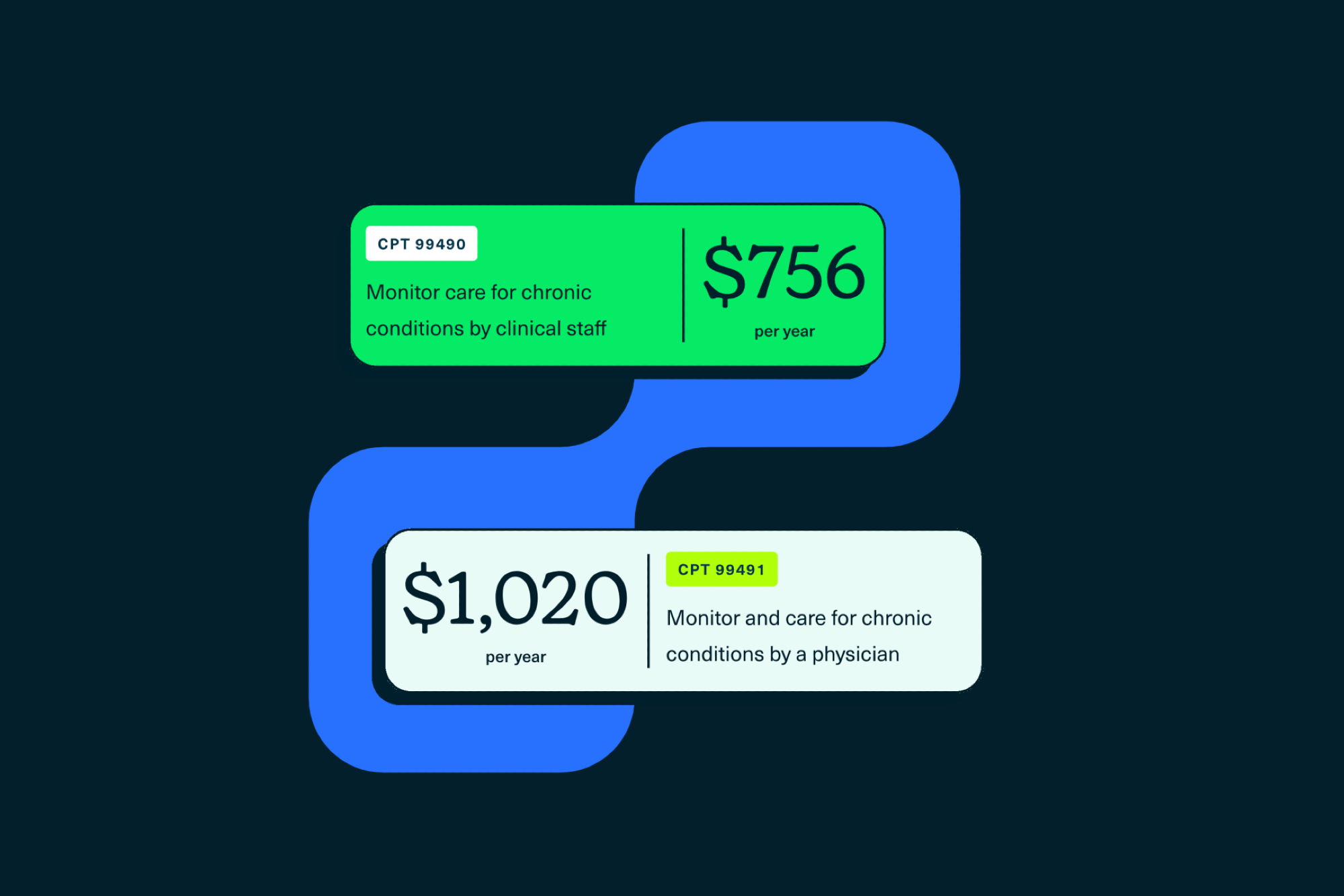
Clinics are not being fully compensated for the check-ins, symptom monitoring, and preventative efforts between office visits. This can stem from multiple factors: not diligently tracking the time spent on these billable encounters, a lack of awareness regarding applicable CPT codes for CCM, and insufficient staff and digital infrastructure to take advantage of eligible CPT codes. A 2020 study found that even with the increased use of CCM by clinics, newer billing codes make up a small proportion. Remote Chronic Care Management (CCM) stands out as a promising solution for this missed potential, offering a structured approach to ensure that clinics harness the full financial potential of their ongoing patient care endeavors.
CCM in action
As a Medicare initiative tailored for improving health outcomes for patients with multiple chronic conditions, Chronic Care Management (CCM) prioritizes personalized care plans and streams of patient-physician communication.
Strategically integrating a remote CCM system offers a solution to meet rising patient demands and seizes eligible reimbursement for services they are already providing. On top of this, it allows clinics to improve clinical decision making and quality of care through more diligent, automated patient check-ins. For example, CCM facilitates symptom monitoring through check-ins, enhances medication adherence, and provides a channel for answering routine patient questions. A robust CCM platform includes services within the scope of related CPT codes, diligently tracking time and integrating notes seamlessly into the EHR system. If powered by generative AI, the system interprets and responds to queries, all while ensuring EHR integration and strict security measures.
How can a digital CCM platform help clinics claim eligible reimbursement opportunities that would otherwise be missed? By automating tracking time spent on calls and chats with patients in real-time and utilizing informed CPT codes, clinics can perform their existing duties without the stress of documentation. With seamless documentation, time tracking, and billing, the right comprehensive CCM platform equips practices to capitalize on their existing clinical services and create opportunities towards financial growth.
Transitioning to CCM can be daunting. However, selecting the appropriate Chronic Care Management software and integrating it with clinic workflows can yield long-term gains for short-term efforts. By embracing CCM, healthcare providers can enjoy an enhanced patient experience, while increasing revenue potential.
Looking to start or scale your remote chronic care management program? Quadrant Health offers a comprehensive, fully-EHR integrated CCM platform for patient communication, care coordination, and clinical documentation, supported by industry-leading generative AI. Request a demo here.
Learn more about how to start a CCM program here.
Learn more about what conditions qualify for CCM here.