Can AI Assisted Care Management Prevent Burnout While Improving Patient Outcomes?
The US healthcare system has experienced high costs, suboptimal outcomes, and a range in the quality of care delivered to patients. Over the past few decades, the US healthcare system has continually faced challenges associated with access to care, variable quality, and increasing healthcare costs.
According to the Centers for Disease Control and Prevention, chronic diseasea is the leading cause of death and disability in the United States accounting for over $4 trillion in annual healthcare costs with 6 in 10 adults having one chronic disease and 4 in 10 adults have at least two chronic diseases.1
However, spending during this time period has not resulted in progression toward better health outcomes, especially for chronic conditions. These challenges are compounded by the fact that 67% of physicians reported burnout and 72% reported emotional exhaustion due to their work.2
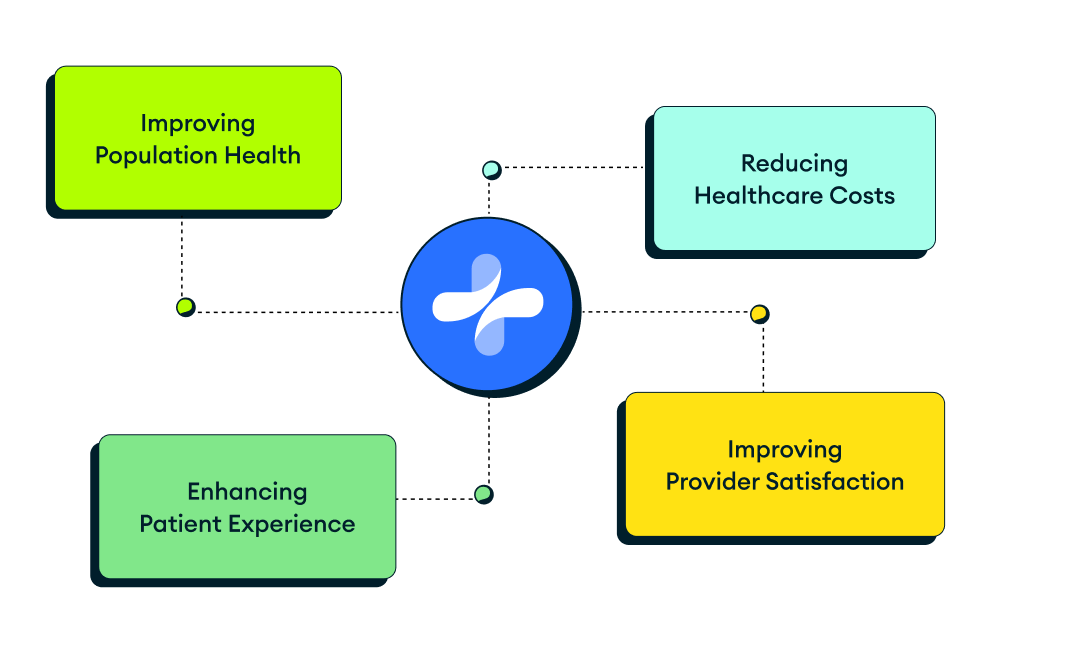
Significant opportunities exist within the healthcare industry to solve these challenges and improve health outcomes by effectively managing costly chronic conditions. Improving on all Quadruple Aim components will certainly help move our communities toward better health, improved experiences, higher satisfaction, and lower costs.
aChronic disease includes heart disease, cancer, chronic lung disease, stroke, Alzheimer’s disease, diabetes, and chronic kidney disease.
AI assisted Care management programs allow providers to effectively manage complex and chronic medical conditions. Patients with chronic and comorbid conditions often need varying levels of care. As a result, enrolling patients into the Centers for Medicare & Medicaid Services Chronic Care Management and Principal Care Management programs have helped providers improve care coordination, reduce hospitalizations, and save healthcare costs.3
These care management programs offer a model of care that is focused on addressing specific issues related to chronic conditions, coordination of care, and developing a comprehensive care plan to achieve health goals.
These programs have been increasing in size4 and a growing body of evidence suggests that individuals in care management programs have a lower rate of readmissions to hospitals and better outcomes.
Recent research has suggested that care management programs improve communication and lower hospital readmissions. In one study with embedded care plans and collaborative care conferences, interprofessional communication was improved across the care continuum for heart failure patients.5
Moreover, hospital admissions decreased by 62% and length of stay decreased by 73%. These results suggest that care management programs are effective at helping patients avoid costly hospital visits and improving communication.
Other research investigating patients with diabetes showed better A1c control and an increase in patients meeting their blood sugar clinical targets.
Similarly, better outcomes were seen in patients with obesity with a greater proportion of weight loss compared to controls.6 Overall, providers reported that care management programs improve treatment adherence, satisfaction, care coordination, and access to the healthcare team.7
Incorporating AI and digital technology can further improve care management programs. Recent advances with generative artificial intelligence (AI) in products such as OpenAI’s chatGPT have created potential to leverage computing to increase efficiency, reduce provider burnout, improve health outcomes, and increase satisfaction with the healthcare system.
Bringing together the power of AI assisted care management programs through applications such as asynchronous patient communication and auto-generating clinical documentation will help drive efficient healthcare at a lower cost to the system and patient.
Automated asynchronous patient communication can help reduce administrative burden for providers and keep patients engaged in their care. The COVID-19 pandemic led to a 63-fold increase in Medicare visits conducted through telehealth in 2020 (from approximately 840,000 visits in 2019 to 52.7 million visits in 2020).8
Regardless of the pandemic, asynchronous care options allow patients to conveniently access providers, save time, reduce their travel burden to the office while still maintaining patient-healthcare professional relationships. These benefits, combined with advancements in technology, have led to increasing demand by patients for asynchronous care over the past few years.
Using AI to help autogenerate intelligent clinical and history seeking questions can help providers maximize the use of their time and increase access to patient-centered care. Reducing manual entry by providers can help speed up diagnosis and improve the experiences of providers. Indirectly, this may decrease burnout and issues that providers have with increasing administrative and non-clinical work.
Similarly, using AI to auto-generate clinical documentation allows providers to easily obtain access to critical data elements that are needed during the provision of care rather than spending time entering data into their clinical systems.
Using algorithms to generate clinically relevant documentation that is dependent on what the patient communicates will help support providers to efficiently diagnose and recommend appropriate treatments or care plans.
Reducing administrative burden is critical for reducing provider burnout, improving experiences, and maintaining a healthy workforce.
Addressing concerns with AI will help build trust among patients, providers, and the larger healthcare community. AI allows providers to save time so they can focus on higher priority activities, however, privacy and security concerns with health data exist.
Additionally, data quality and bias may affect overall trust among providers and patients who interact with AI tools. Addressing the following 3 concerns will help build trust among patients, providers, and the broader healthcare community:
- Maintaining the privacy and security of health data is extremely important. AI platforms should always integrate an added layer of security to protect health data to avoid breaches or inadvertent disclosure of personal health information.
- Algorithms are only as good as the data they use (garbage in = garbage out). Variable data quality remains a concern alongside potential bias of algorithms that run on data that are biased. AI programs should always consume high quality data using unbiased algorithms.
- Building trust among providers and patients with AI tools is paramount for successful implementation. With any new technology, building trust and creating transparency is key to further adoption. Ongoing communication and education to providers, patients, and the broader healthcare community will help maintain transparency, manage expectations, and build trust.
Ongoing investments are critical for laying the groundwork that will further embed AI within the healthcare industry.
The promise of AI is rooted in creating efficiency and reducing work burden and this has the potential to yield substantial benefits for our future and collective health. But just as important, our experiences with the healthcare system will improve and providers will go back to doing what they were initially trained to do: address medical conditions, improve outcomes, and take care of the health of their patients.
Quadrant Health is an AI-driven comprehensive CCM platform that allows practices to personalize and perform patient care plans. Learn more here or request a demo here.
REFERENCES
- Centers for Disease Control and Prevention. Chronic diseases in America. Accessed on July 7, 2023.
- Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA. Prevalence of burnout among physicians: a systematic review. JAMA. 2018 Sep 18;320(11):1131-1150. doi: 10.1001/jama.2018.12777.
- Shurrer J, O'Malley A, Wilson C, McCall N, Jain N.. Evaluation of the diffusion and impact of the chronic care management (CCM) services: final report. Princeton, NJ: Mathematica Policy Research, 2017.
- Reddy A, Marcotte LM, Zhou L, Fihn SD, Liao JM. Use of chronic care management among primary care clinicians. Ann Fam Med. 2020 Sep;18(5):455-457. doi: 10.1370/afm.2573.
- Koutlas A, Jenkins P. Reducing hospital admissions for patients with heart failure by implementing the chronic care management framework: a cost, quality and satisfaction improvement project. J Dr Nurs Pract. 2022 May 16:JDNP-2021-0019.R1. doi: 10.1891/JDNP-2021-0019.
- Holtrop JS, Luo Z, Piatt G, Green LA, Chen Q, Piette J. Diabetic and obese patient clinical outcomes improve during a care management implementation in orimary care. J Prim Care Community Health. 2017 Oct;8(4):312-318. doi: 10.1177/2150131917715536.
- O'Malley AS, Sarwar R, Keith R, Balke P, Ma S, McCall N. Provider experiences with chronic care management (CCM) services and fees: a qualitative research study. J Gen Intern Med. 2017 Dec;32(12):1294-1300. doi: 10.1007/s11606-017-4134-7.
- Office of the Assistant Secretary of Planning and Evaluation. Medicare beneficiaries’ use of telehealth in 2020: trends by beneficiary characteristics and location. Accessed on July 13, 2023.